History of the Department
by James P. Neifeld, MD, FACS, Professor Emeritus
In 1837, Dr. Augustus Warner, a graduate of the University of Maryland who was on the surgical faculty at the University of Virginia, became disillusioned with the clinical material available and felt that Richmond would provide a much broader patient base. He organized a petition to have Hampden-Sydney College put a medical college in Richmond.
Dr. Warner became the first Professor of Surgery, as well as Dean when the institution opened in 1838. He was known for being a superb surgeon, performing a partial mandibulectomy in nine minutes! The first permanent building was the Egyptian Building, which opened in 1845 and is still being used as a building for the Medical School. This was the first permanent hospital of the Medical College of Virginia and had well ventilated wards and private rooms.
Dr. Warner died in 1847 (probably of appendicitis) and was succeeded by Dr. Charles Bell Gibson. Dr. Gibson was also a well known surgeon and was one of the first surgeons to use anesthetics. He wrote on femoral artery ligation, treatment of femur dislocations, and resection of a maxillary sarcoma. In 1861 the Commonwealth of Virginia organized its military forces with a medical department under Dr. Gibson as Surgeon General. He died in 1865.
At the time of the secession of the South, there were many Southerners attending medical schools in the North. A large group was in Philadelphia. Hunter Holmes McGuire led a group of 150 medical students to Richmond, many of whom transferred to the Medical College of Virginia.
Hunter McGuire was well known and thought to have been a major figure for the medical establishment during the Civil War, but he was actually quite junior. His wartime notoriety derives from the amputation of the arm of Stonewall Jackson and his subsequent demise (probably from pneumonia).
Dr. James McCaw, who served MCV for about 50 years, planned and organized the largest hospital that ever existed in the western world. Chimborazo Hospital was located just east of the Medical College of Virginia campus and was said to have had as many as 7000 beds. It had one of the lowest mortality rates of any hospital in the Civil War. The buildings were ventilated and accommodated 40 to 60 patients. There were also approximately 100 tents with eight to ten soldiers or convalescent patients per tent. Over 76,000 patients passed through this hospital and 7000 died, an exceptionally good record for the time.
MCV was the only southern medical school to remain open throughout the Civil War. The fire that burned much of Richmond at the end of the war did not affect MCV. Learn more about Civil War Hospitals in Richmond.
After the war, Dr. McGuire practiced in Richmond and became closely associated with MCV. He became the third Professor of Surgery in 1865. He was one of the first surgeons to practice Listerism, the first to perform a suprapubic cystostomy, and he reported ligation of the abdominal aorta. Despite a busy private practice he was always willing to treat charity cases and treated Confederate soldiers without charge. He is one of the very few to be President of the American Surgical Association, Southern Surgical Association, and American Medical Association. He was Professor of Surgery until 1881 but resigned following a fight with the Board of Trustees. After his resignation, he founded St. Luke’s Hospital and in 1892 his interest in teaching led him to help found a new medical school, the University College of Medicine. This medical school developed a faculty better than MCV’s and the curriculum was extended to three years.
The fourth Chairman of Surgery at MCV was appointed in 1881: Dr. John Dorsey Cullen. He was said to have been a skillful surgeon and an excellent teacher. He published on hepatic abscess, traumatic tetanus, and diseases of the bones. After his death in 1893, George Ben Johnston became the next Professor of Surgery. He was also an advocate of Listerism and published on nephrectomies, imperforate anus, renal and hepatic diseases, and biliary surgery. He became President of the Southern Surgical Association and the American Surgical Association. During his time as Chairman, MCV became the first medical school in Virginia to require a four-year term. Following the Flexner Report, Dr. Johnston and Dr. Stuart McGuire, then President of the University College of Medicine, merged the two medical schools in 1913 to form the new Medical College of Virginia.
Dr. Stuart McGuire, son of Dr. Hunter McGuire, was an eminent surgeon in his own right and was chosen Dean of the Faculty. Dr. Johnston died in 1916 and Dr. McGuire took over as Chair of Surgery. He became known for his publications on toxic goiter, cholecystitis, and appendicitis. He was said to be an outstanding organizer and teacher.
During this period of time World War I was raging in Europe and it was decided to organize a Red Cross Hospital in Richmond based on MCV. Dr. Stuart McGuire helped organize this unit. He was the first Director of this unit, was replaced on a temporary basis by Major Alexander Williams, but after the unit went to France, Dr. McGuire resumed his position as Director. Base Hospital No. 45, as it was known, was supposed to be far behind the front lines but it actually was within a few miles of the front lines and served not just as a base hospital but as a triage and evacuation hospital. Within two weeks of a major United States offensive in September, 1918, 8000 casualties arrived. The mortality rate was one of the lowest of any of the military hospitals of that time; Dr. McGuire was awarded the French Medal of Honor as well as the Distinguished Service Cross from the United States Government.
Following the war, Dr. McGuire became President of MCV. In that position he had to give up being Professor of Surgery and Dr. Murat Willis succeeded him. Dr. Willis had a busy clinical practice, apparently was rarely at MCV, and most of the teaching was done by Dr. Paul LaRoque. Dr. LaRoque arrived in Richmond in 1905 to join the faculty of the University College of Medicine. He was a prolific writer on many subjects including pelvic surgery, vascular surgery, and intestinal obstruction, but his major contribution was in the field of hernia surgery. He died suddenly in 1934.
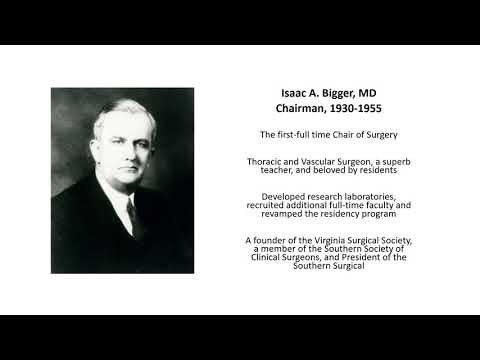
One of the critical problems the Medical School faced was the lack of a full time faculty. Dr. Isaac A. Bigger was appointed as the first full-time Chair of Surgery in 1930. He was one of the most beloved men of his time. His primary contributions were in thoracic and cardiovascular surgery. He was the first to resect a pulmonary bleb, which is responsible for spontaneous pneumothorax. The repair of tracheo-esophageal fistulae was another major interest of his and he accomplished one of the first major series of successful heart wound repairs. He co-edited a very successful operative surgery textbook into a sixth edition with Dr. Guy Horsley. Dr. Bigger was President of the Southern Surgical and was instrumental in the formation of the Virginia Surgical Society. During Dr. Bigger’s 25 years as Chairman of the Department of Surgery, research laboratories, a better defined residency program, and excellence in clinical care all developed.
Dr. Everett Evans was a brilliant faculty member recruited by Dr. Bigger to develop burn wound care. The Burn Unit was the first civilian intensive care unit in the United States and the first burn formula for fluid replacement was developed under Dr. Evans’ leadership.
When World War II was imminent, military hospitals were again based on individual university and large private hospitals. Dr. McGuire was asked to reorganize Base Hospital No. 45 as the 45th General Hospital but due to age and poor health he asked Dr. Carrington Williams to take over. The surgical services were organized into General Surgery and other services under the overall leadership of Dr. Guy Horsley. The Unit served with distinction in North Africa and Italy and a large number of MCV physicians and nurses made names for themselves. The Unit established the first blood bank in a military hospital in March, 1944, and soon averaged about 430 units transfused per month. Secondary wound closure (at day four to five) was pioneered in this unit, fibrin sealant was first used for brain surgery and hepatic hemorrhage, primary nerve repair was developed as was a method of rapid blood acquisition. These advances were soon used throughout all military hospitals.
After World War II, people returned home and the Department of Surgery continued to flourish under Dr. Bigger until his death in 1955. In 1956, a young surgeon from Boston, David Hume, was named Chairman of the Department of Surgery. Dr. Hume became the beneficiary of one of the largest NIH grants ever awarded to that time, over six million dollars, and developed a transplant program at MCV. His research included work in transplantation, endocrinology, vascular, and bariatric surgery. He mapped the hypothalamus and published seminal papers on pheochromocytomas and parathyroid disease. He helped describe the use of azothioprine, steroids, and total body irradiation for immunosuppression. Dr. Hume was a revered figure, superb teacher and developed an incredible faculty.
Dr. Jim Brooks, a pioneer in thoracic surgery, Dr. Arnold Salzberg, a pioneer in pediatric surgery, and Dr. Richard Lower, who developed the technique of heart transplantation in animals, were members of the faculty. Dr. B. W. Haynes became Director of the Burn Unit and Dr. Walter Lawrence, Jr., an eminent surgical oncologist, founded the first Division of Surgical Oncology at any university hospital. Many leaders in transplantation and other leaders in American surgery were trained under Dr. Hume’s tutelage.
In 1973, Dr. Hume died in a plane crash in Southern California. Dr. Lawrence was the Interim Chairman until the arrival of Dr. Lazar Greenfield in 1974. Dr. Greenfield headed the Department for 12 and one-half years. He provided a great deal of stability, had a major interest in thrombo-embolic disease, and worked closely with Thoracic Surgery, Vascular Surgery, and Cardiac Surgery. Dr. Greenfield hired a large number of faculty and both research and clinical care continued to flourish. In 1986, Dr. Greenfield left to become Chair of Surgery at the University of Michigan in Ann Arbor.
Dr. Andrew Wechsler was recruited from Duke in 1988, and brought very much of a business atmosphere to the Department. Dr. Ronald Merrell was recruited from Yale in 1999, and during his brief tenure the Hume-Lee Transplant Unit and the Evans-Haynes Burn Unit became realities. In 2003, Dr. Merrell resigned as Chairman and Dr. James Neifeld became Chairman of the Department of Surgery. During the next three years, many faculty were hired in the Department both in clinical and research positions, teaching was revamped, and the administrative aspects of the Department were enhanced to meet current requirements. Then in August 2014, Dr. Neifeld retired and Dr. Vigneshwar Kasirajan, former Chair of the Division of Cardiothoracic Surgery, was appointed new Chair of Surgery and continues in this position today.
Surgery Research
The Department has jumped from 42nd to 27th nationally in NIH funding and continues to develop multidisciplinary discoveries across campuses to further expand our clinical and research activities.